**Medical Uses and Forms:**
– Oxycodone is used to manage moderate to severe acute or chronic pain and improve quality of life in certain pain types.
– It is available in immediate-release and controlled-release formulations, with various combinations with other drugs.
– The controlled-release tablet is effective for 12-hour intervals and is recommended as a second-line alternative to morphine for cancer pain.
– Liquid solutions with specific concentrations are available, and parenteral formulations are used outside the US.
**Side Effects and Dependence:**
– Common side effects of oxycodone include constipation, nausea, vomiting, dizziness, and itching.
– Chronic use may lead to severe constipation issues, with formulations developed to address opioid-induced constipation.
– Abrupt discontinuation of oxycodone can lead to severe withdrawal symptoms, necessitating gradual withdrawal for regular users.
– Recreational or high-dose users are at higher risk of severe withdrawal, with reported symptoms in newborns of mothers using oxycodone.
**Hormone Levels and Interactions:**
– Chronic use of oxycodone may lead to low sex hormone levels, with higher doses increasing the risk of hypogonadism.
– Interactions with CYP3A4 and CYP2D6 enzymes can alter oxycodone clearance, with varying effects from inhibitors and inducers of these enzymes.
– Genetic variation in these enzymes influences oxycodone metabolism, with specific drugs affecting oxycodone plasma concentrations.
**Pharmacology and Pharmacokinetics:**
– Oxycodone is a selective full agonist of the μ-opioid receptor, with low affinity for other opioid receptors.
– It inhibits neurotransmitter release by decreasing cAMP production and has specific affinities for MOR.
– Oxycodone’s pharmacokinetics vary based on routes of administration, formulations, and onset times for pain relief.
– The drug’s chemistry, biosynthesis, and detection in biological fluids play a role in its pharmacological profile.
**History, Development, and Regulation:**
– Oxycodone was first synthesized in 1916 and introduced to the US market in 1939 for pain management.
– Historical use of oxycodone includes its recognition as a “Miracle Drug” and its military use for battlefield analgesia.
– The drug’s regulation as a Schedule II controlled substance and the development of OxyContin by Purdue Pharma in 1995 are key milestones.
– OxyContin’s impact, revenue generation, and role in the opioid epidemic, including abuse and overdose deaths, are significant aspects of its history and current status.
Oxycodone, sold under various brand names such as Roxicodone and OxyContin (which is the extended release form), is a semi-synthetic opioid used medically for treatment of moderate to severe pain. It is highly addictive and is a commonly abused drug. It is usually taken by mouth, and is available in immediate-release and controlled-release formulations. Onset of pain relief typically begins within fifteen minutes and lasts for up to six hours with the immediate-release formulation. In the United Kingdom, it is available by injection. Combination products are also available with paracetamol (acetaminophen), ibuprofen, naloxone, naltrexone, and aspirin.
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ɒksiˈkoʊdoʊn/ |
| Trade names | OxyContin, Endone, others |
| Other names | Eukodal, eucodal; dihydrohydroxycodeinone, 7,8-dihydro-14-hydroxycodeinone, 6-deoxy-7,8-dihydro-14-hydroxy-3-O-methyl-6-oxomorphine |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682132 |
| License data | |
| Pregnancy category |
|
| Dependence liability | High |
| Addiction liability | High |
| Routes of administration | By mouth, sublingual, intramuscular, intravenous, intranasal, subcutaneous, transdermal, rectal, epidural |
| Drug class | Opioid |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | By mouth: 60–87% |
| Protein binding | 45% |
| Metabolism | Liver: mainly CYP3A, and, to a much lesser extent, CYP2D6 (~5%); 95% metabolized (i.e., 5% excreted unchanged) |
| Metabolites | • Noroxycodone (25%) • Noroxymorphone (15%, free and conjugated) • Oxymorphone (11%, conjugated) • Others (e.g., minor metabolites) |
| Onset of action | IR: 10–30 minutes CR: 1 hour |
| Elimination half-life | By mouth (IR): 2–3 hrs (same t1/2 for all ROAs) By mouth (CR): 4.5 hrs |
| Duration of action | By mouth (IR): 3–6 hrs By mouth (CR): 10–12 hrs |
| Excretion | Urine (83%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.874 |
| Chemical and physical data | |
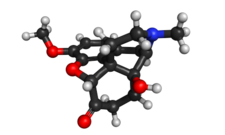
| Formula | C18H21NO4 |
| Molar mass | 315.369 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 219 °C (426 °F) |
| Solubility in water | 166 (HCl) |
| |
| |
| (verify) | |
Common side effects include euphoria, constipation, nausea, vomiting, loss of appetite, drowsiness, dizziness, itching, dry mouth, and sweating. Side effects may also include addiction and dependence, substance abuse, irritability, depression or mania, delirium, hallucinations, hypoventilation, gastroparesis, bradycardia, and hypotension. Those allergic to codeine may also be allergic to oxycodone. Use of oxycodone in early pregnancy appears relatively safe. Opioid withdrawal may occur if rapidly stopped from withdrawal. Oxycodone acts by activating the μ-opioid receptor. When taken by mouth, it has roughly 1.5 times the effect of the equivalent amount of morphine.
Oxycodone was originally produced from the opium poppy opiate alkaloid thebaine in 1916. It was first used medically in Germany in 1917. It is on the World Health Organization's List of Essential Medicines. It is available as a generic medication. In 2021, it was the 59th most commonly prescribed medication in the United States, with more than 11 million prescriptions. A number of abuse-deterrent formulations are available, such as in combination with naloxone or naltrexone.
